Africa’s Lowest Cost AIDS Prevention Strategy?
A new paper from PLOS NTDs suggests mass drug administration (MDA) for schistosomiasis represents a highly cost-effective and even cost-saving approach for reducing HIV transmission in Africa.
Over the years I have written a lot (and beaten the drum pretty hard) about the importance of female genital schistosomiasis (FGS), its devastating effects on young women, and its key role in promoting HIV/AIDS transmission in Africa. FGS occurs when the eggs of Schistosoma haematobium are deposited in the uterus, cervix, and vagina of girls and women living in the major affected areas located in southeastern Africa and Francophone West Africa and Nigeria. A number of clinical studies have documented how the trapped eggs and resulting granulomas cause pain and contact bleeding, and ultimately shame, marital discord, and even depression. Two independent epidemiological studies (led by groups from Oslo and Weil Cornell Medical College) have linked FGS to multifold increases in acquiring HIV. While the exact mechanism for this is still unclear, presumably the schistosome eggs and granulomas produce sufficient ulceration and bleeding to facilitate virus entry leading to HIV infection.
FGS is by no means rare and in a recent Speaking of Medicine post I estimated that between 20 and 150 million African girls and women suffer from this condition. I also argued that FGS may be the most common gynecologic condition in Sub-Saharan Africa, which few are willing to talk or write about.
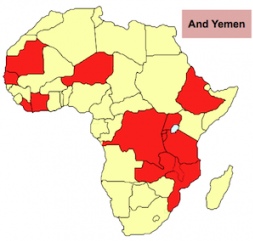
The very good news is that FGS could potentially be prevented if we reach girls and treat them early enough in life with praziquantel. In Africa praziquantel is typically administered through annual MDA campaigns conducted by African health ministries, with logistical and technical assistance from the London-based Schistosomiasis Control Initiative (SCI) now operating in about a dozen African countries (Fig. 1) (although other organizations, including RTI International, FHI 360, HKI and Carter Center, are also involved in Africa), together with the World Health Organization and its Regional Office for Africa (AFRO). USAID, DFID-UKAID, and a private END (Ending Neglected Disease Fund) provide important financial support for these activities, with advocacy from a Global Network for NTDs.
A critically important piece of information is that schistsomiasis MDA is ridiculously inexpensive because of generous praziquantel donations from Merck KGaA or (when there is insufficient drug being donated) it can be provided as an extremely low-cost generic (often averaging around 8 cents per tablet) from Shin Poong, MedPharm and other companies through UNICEF, WHO, and the World Bank.
Now a paper just out in PLOS Neglected Tropical Diseases gives us compelling reasons to recast schistosomiasis MDA as a back door AIDS prevention strategy. A group led by Yale University’s Martial L. Ndeffo Mbah and Alison Galvani focused on the nation of Zimbabwe to determine that by preventing HIV transmission schistosomiasis MDA targeting school-aged children would save up to US$100 million in AIDS healthcare costs in that country over a ten year period. Moreover, they determined that MDA for schistosomiasis is actually more cost-effective as an intervention to block HIV transmission than better known approaches such as male circumcision or the treatment of other sexually transmitted diseases. It is more cost-effective than antiretroviral therapy as a means to prevent new HIV infections.
Thus, in many respects organizations such as SCI and WHO together with African health ministries are actually leading low-cost HIV/AIDS prevention efforts in Africa and have been doing so for the last decade!
For me, a key take home message is that the major organizations committed to HIV/AIDS prevention in Africa, such as PEPFAR and the Global Fund to Fight AIDS, TB, and Malaria, as well as the ONE Campaign, must embrace schistosomiasis MDA and support its expansion throughout the affected areas of Africa in order to prevent or reduce the burden of FGS. In the meantime a few R&D groups, including our Sabin Vaccine Institute PDP, are also working to develop a schistosomiasis vaccine as an innovative biotechnology to potentially eliminate schistosomiasis from Africa and therefore prevent AIDS in southeastern and Francophone West Africa.
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin:0in;
mso-para-margin-bottom:.0001pt;
mso-pagination:widow-orphan;
font-size:10.0pt;
font-family:”Times New Roman”,”serif”;
mso-fareast-language:EN-US;}

[…] New commentary on the PLoS Speaking of Medicine Blog from Dr. Peter Hotez, president of the Sabin Vaccine Institute, highlights exciting findings that “give us compelling reasons to recast schistosomiasis MDA as a back door AIDS prevention strategy.” […]